Skip the confusion. Get honest answers and personalized solutions from someone who’s been there.
Call Yvonne!
954-646-3666
Let’s find coverage that fits your life and budget. I’ll show you all your options – and potential savings – with no obligation.

Group health insurance provides comprehensive coverage for multiple people under a single policy, offering economies of scale and enhanced benefits that individual plans often cannot match. Whether you’re a business owner looking to provide employee benefits, part of a professional association, or exploring group options through other organizations, group health insurance delivers cost-effective coverage with valuable benefits for all members.
At Heaven Insurance Consultants, we understand that South Florida organizations need group health insurance solutions that provide excellent coverage while managing costs effectively. That’s why we specialize in helping businesses, associations, and groups discover health insurance plans that meet the diverse needs of their members while delivering exceptional value and comprehensive protection.
Understanding group health insurance requires expertise in plan design, compliance requirements, and group dynamics that create successful benefits programs.
We provide comprehensive education about group health insurance options and how group coverage differs from individual plans. Our team stays current with group insurance regulations, plan offerings, and industry best practices to ensure you receive expert guidance for your group coverage decisions.
Understanding group needs requires evaluating member demographics, budget parameters, and coverage objectives. We help you analyze group health insurance options that provide valuable benefits for members while achieving cost efficiency and meeting organizational goals.
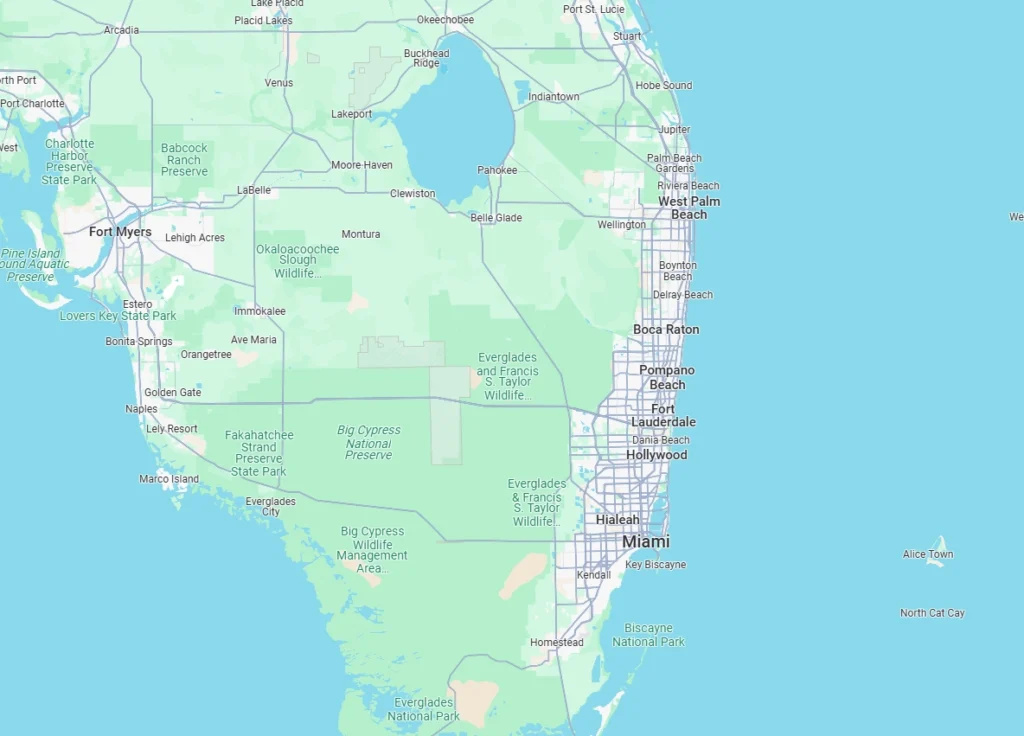
As your trusted South Florida insurance consultants, Heaven Insurance Consultants understands the group insurance marketplace in Palm Beach County and surrounding areas. We know which carriers offer competitive group rates, which plans provide strong local networks, and how coverage works with area healthcare providers.
We believe in providing thorough education about group health insurance benefits and how group coverage works for organizations and members. Our goal is to ensure your expectations are met in a meaningful, clear manner, so you understand the advantages and responsibilities of group health coverage.
Our efficient approach helps you design group health insurance programs that balance comprehensive benefits with cost management. We analyze different coverage options, contribution strategies, and plan features to create group programs that work for both the organization and its members.
Our relationship doesn't end when you enroll. We provide year-round assistance whenever you have questions about your group coverage, need help with member enrollment issues, or want guidance on plan modifications and annual renewals.
We make getting insured simple with a fast, no-fuss process. While we handle the details, you stay informed every step of the way - so you get coverage without waiting.
We’re always available to assist you - day or night. From coverage questions to claims help, our team provides prompt, professional support whenever you need it.
Group health insurance is coverage purchased by an organization to provide health benefits to its members, employees, or participants. These plans leverage the collective buying power of the group to achieve better rates and benefits than individuals could typically obtain on their own.
Cost Effectiveness
Enhanced Benefits
Employers and Businesses
Associations and Organizations
Group health insurance comes in various formats designed to meet different organizational needs, member preferences, and budget requirements.
Fully Insured Group Plans
Benefits of Fully Insured Plans
Self-Funded Group Plans
Benefits of Self-Funded Plans
Coordinated Care Model
HMO Plan Benefits for Groups
Flexible Network Model
PPO Plan Benefits for Groups
Consumer-Directed Healthcare
HDHP Benefits for Groups
Group health insurance must comply with various federal and state regulations that affect plan design, member rights, and organizational responsibilities.
Affordable Care Act (ACA) Provisions
ERISA Requirements
50+ Employee Requirements
Penalty Calculations
Creating successful group health insurance requires balancing member needs, organizational budget, and compliance requirements.
Member Characteristics
Organizational Factors
Coverage Level Options
Member Choice Strategies
Premium Contribution Models
Cost Control Mechanisms
Effective group health insurance requires ongoing administration to ensure smooth operation and member satisfaction.
Initial Enrollment
Ongoing Administration
Member Education
Ongoing Communication
Group health insurance spreads risk across multiple people, typically resulting in lower costs and better benefits than individual coverage. Group plans offer guaranteed issue coverage regardless of health status, often include employer contributions, and provide access to larger provider networks.
Most group health insurance requires a minimum of 2-5 eligible participants, though requirements vary by state and insurance carrier. Some association plans and special group arrangements may have different minimum participation requirements.
Eligibility depends on the type of group and plan rules. For employer plans, typically full-time employees and their dependents are eligible. Association plans may be available to members in good standing, while other group arrangements have specific eligibility criteria.
Group health insurance costs vary based on group size, member demographics, plan type, and coverage levels. Costs are typically shared between the organization and participants, with the organization often paying a significant portion of premium costs.
Some group health insurance programs offer multiple plan options, allowing members to choose coverage that best fits their needs and budget. Other groups offer a single plan option to maximize purchasing power and simplify administration.
When members leave the group, they typically lose coverage at the end of the month or their last day of eligibility. They may be eligible for COBRA continuation coverage or special enrollment in individual marketplace plans.
Yes, group health insurance plans cannot exclude coverage for pre-existing conditions or charge higher rates based on health status. Coverage for pre-existing conditions begins when the member's coverage becomes effective.
Group health insurance plans typically have annual renewal periods when changes can be made. Some changes may be possible during the year due to qualifying events, but major plan changes usually occur at renewal.
Group plans must comply with various federal and state regulations, including ACA requirements, ERISA provisions, and state insurance laws. Large employers may have additional requirements under the employer mandate.
Group health insurance administration includes initial enrollment, ongoing eligibility management, life event processing, and annual open enrollment. Many organizations work with benefits administrators or insurance brokers to manage these processes effectively.

Don’t let complex group health insurance decisions overwhelm your organization. Heaven Insurance Consultants specializes in helping South Florida organizations understand their group health insurance options and design programs that provide excellent member benefits while managing costs effectively.
Our group health insurance expertise includes:
Don’t risk choosing group coverage that doesn’t meet your members’ needs or your budget requirements. Contact Heaven Insurance Consultants today to explore group health insurance options and build a program that delivers value for your organization and its members.
Ready to provide excellent group health benefits? Contact Heaven Insurance Consultants ☎️ +1 (954)646-3666 for your free group health insurance consultation and program design analysis.
Heaven Insurance Consultants proudly helps organizations throughout South Florida understand and implement comprehensive group health insurance programs. Our expertise in group insurance and deep understanding of Palm Beach County’s business and organizational landscape ensures you receive expert guidance tailored to your group’s unique needs.
We serve businesses, associations, and organizations in Boynton Beach, Delray Beach, Boca Raton, West Palm Beach, Wellington, Lake Worth Beach, Lantana, Ocean Ridge, and surrounding South Florida communities. Our local knowledge helps you design group programs that work with area healthcare providers and meet your organization’s objectives.
Contact us today to learn why South Florida organizations trust Heaven Insurance Consultants for their group health insurance needs and comprehensive benefits program design.